Please note I’m not a doctor, nor do I play one on television. I’m just related to several of them, even though they’d rather be neutering cats than dealing with fickle, litigation-prone humans. That being said, this post is solely my personal experience and probably wasn’t a good idea in the first place.
At long last, it seems that the sun of post-pandemic life has broken through the hazy greenish clouds of COVID-19. Christine, laid up now for almost a year with chronic back and neck pain with a side of tinnitus since our wedding party and Türkiye trip last June, was feeling cautiously optimistic about being on airplane seats again, and our good friends Branden and Caitlin were also looking to travel. The two of them had never been to Mexico before, so with the additional of our friend Dan, we made a five-some plan to travel to Tulum, just a few hours south of Cancun where Christine and I had last been in December 2021, right after our wedding.
Everything seemed like it would be in good order until, a mere week before we were supposed to fly out of Chicago on March 20th – my left lung collapsed. Again. For the third time in four months. Christine and I had both (finally) had our first and hopefully only coronavirus cases in November 2022 and I was suspicious that lingering viral whatsits in my body were causing this new and frequent resurgent of collapses. Over the past decade of living with chronic pneumothorax, I’ve become accustomed to about one collapse a year. This was an irritating new pattern starting to emerge.
Not that my collapses are what I (at this point in my life) would call “a big deal.” A dull, mild ache in my back when I lie in certain positions, slightly shortness of breath. I’ve never been diagnosed with a total collapse, either, they’ve always just be in the 15-20% range. And ol’ righty has always been fine, carrying the load for his weaker partner. But all pneumothorax sufferers know that you’re not supposed to fly with a collapsed lung. It’s basically the first thing they tell you (that, and no SCUBA diving) when you join this happy, breathless club. (It’s brought up quite a bit on our subreddit.) How was I going to go to Mexico with my four fellows next week?
Well, I’ve got my trump card, I thought (triumphantly) to myself. I’ll just check myself into the hospital, get put on a pure oxygen nasal cannula overnight, the osmotic pressure of the heavier atmospheric air (nitrogen, carbon dioxide, and oxygen) vs the lighter oxygen in my lungs will cause the air outside my lungs, to get pulled back in, and I’ll be totally cured in a matter of days, and certainly by the 20th. Off to the doctor I go to get a referral!
….Except, the last time I had done this little fast-heal trick had been pre-pandemic. You might have heard there’s a slight oxygen shortage going on worldwide. My doctors apologetically reminded me of this and said that basically you needed to be having serious medical complications in order to be granted oxygen in this day and age. Well, nuts. Even three days after the collapse, I could tell I was on the mend – it was getting less awkward to sleep on my back each night.
At this point, my insurance and I (mostly I) were paying for new x-rays of my chest every couple of days. Finally, on the 20th itself, I had a meeting with a thoracic surgeon to discuss possibly redoing the pleurodesis surgery procedure I had gone through a decade earlier. The surgeon was sympathetic, and we had a good hour long discussion about why he didn’t have high-hopes for a second, similar surgery. It turns out that when your lung tissue is more-or-less glued onto the inside of your chest wall, which is how further pneumothoraxes are prevented, it’s kind of the surgical equivalent of collapsing the entrywide behind you. All of the post-pleurodesis collapses had all been, after all, near the top part of my lung, not my side – which is where the typical entry points for the procedure are (entering from the shoulder is far more complicated because of the greater number of nerves, tendons, and other stuff up there). For all we knew, the “glue” of the previous surgery was still holding strong in my side. If he were to go in again, the process of entering my chest cavity might badly damage my lungs. Not guaranteed, but it would certainly be more risky than the first time.
“So, doc, about flying – of course everyone knows we collapsey types aren’t supposed to fly when we’re having an episode – what’s the worst case scenario?”
He said that the worst case that could happen is that since airplanes are pressurized, and the atmospheric air “bubble” that is trapped in the pleural space between your lungs, and your chest wall, is not able to equalize with the lowered air pressure of the cabin that’s inside your lungs, it could start to swell in your chest, press against your heart, and cause a cardiac arrest situation while you’re on the airplane. That’s about the worst direct occurrence for flying in this condition.
“What if,” I said carefully, “I were to go on an airplane now, with my lung collapse percentage down to just 3-5% and I’m almost healed?”
Ah yes, he said, glancing at his notes. Your primary care provider did mention you had a vacation in Mexico coming up. Well… I won’t speak against official medical guidelines. You’re not supposed to travel with a pneumothorax, of any size, for at least a few days after an x-ray shows it has closed. However, that being said, based on your history of having these collapses, the small percentage it has left to close, and your general overall good health besides this condition, I do think that the likelihood of anything happening like I described… is very low.
“Good enough for me!” I thought.
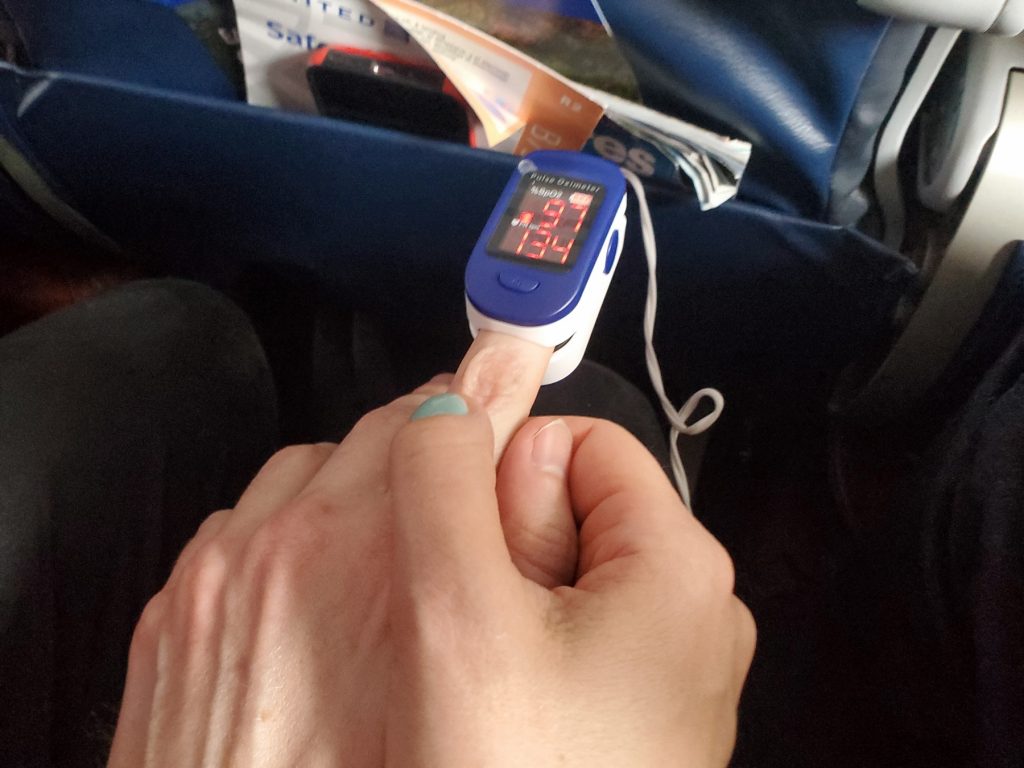
By the time I was actually in the car with Christine, ten minutes away from the parking lot where we’d be catching the Chicago metro to the airport, though, I wasn’t feeling so confident. I popped a half xanax (and had Christine drive) and drifted peacefully through security. On the plane itself, I put on an inexpensive pulse oximeter I’d purchased a few days ago for the trip, and put it on my index finger briefly to get a baseline reading. 97%, not bad at all.
The plane took off. I squeezed Christine’s hand tightly, and she squeezed back.
We looked at the pulse oximeter. It dipped to 96% and stayed there. My heartbeat slowed a bit as I relaxed. I… seemed to be fine. As the plane climbed, I did notice a slight increase in the already very mild remaining soreness of the pneumothorax, an increasing sense of pressure. It did seem likely that the bubble of air outside my lung was indeed expanding somewhat. I wondered vaguely what the math problem would be to determine the volume of air expansion with a human body as the vessel as a pressurized airplane rose in altitude. But that was all.
The pulse oximeter behaved in an odd manner. It did continue to fall, overall, as the plane rose. But Christine put it on as we flew, and my oxygen percentage was always within a point or two of hers. Both of us finally hit a low of 91% while at cruising altitude, but neither of us felt worse for wear. I suppose it makes sense that even in a pressurized cabin, there still would be a lower amount of oxygen to go around, but I was only speculating.
Ironically, it was actually landing and going outside into the humid Yucatan Peninsula air at the Cancun airport that was the worst for me. A few minutes after leaving the airport and waiting for our taxi that would take us to Tulum, I was practically doubled over from a feeling of pressure in my chest. I had been fine inside the airport’s typical air conditioned bland environment, but I did not adjust well to the outdoors. I wondered again if I had made a huge mistake in traveling.
But, over the next couple of hours, the pressure went away again, and I was back to feeling ‘mostly-fine’ like I had before the trip. I still knew I had a return flight to make, so I vowed to really treat myself gingerly and not overexert myself. This would not be a mountain-biking vacation. I still had another flight home in another week, too.
It was a good trip, too. The five of us attended a Yucatanean cooking class with many other tourists, we swam in an open cenote, we laid out on a beach, and visited several very nice restaurants (we particularly enjoyed, and recommend ARCA in the Hotel Zone). A special experience for all of us was a private boat tour Branden planned for us, with a crew of three jovial young men who skippered, cooked, and took the gang out for snorkeling a few miles out from shore. Unfortunately, a few of us, including myself, were feeling a bit seasick from the high speed, somewhat choppy outbound journey, and personally I was content with enjoying the scenery from the bow deck, and having a few beers. (probably shouldn’t have had the margarita right before we took off at what felt like Mach 1).


By the time half the week had passed, the healing seemed to have completed on its own. I no longer felt the tightness in my side or soreness when lying on my back. I still considered to treat myself gingerly for the final few days but I was no longer worried about the flight home. However, I do understand that I was lucky, and I definitely don’t want to make a habit out of this. I understand why the pulmonary specialists have lines in the sand like “any % collapse, flying forbidden” as I’m sure liability-wise it makes sense. But I guess after over twelve years of dealing with this, I was just tired of chronic pneumothorax getting its way in how I run my life.


No one has commented on this post - please leave me one, I love getting feedback!
Follow this post's comments, or leave a Trackback from your site